Prostate Cancer Awareness
When it comes to the prostate, people often think of two things: procreation and pleasure. Other than that, though, there isn't much health-related knowledge available regarding this sexually significant part of the body.
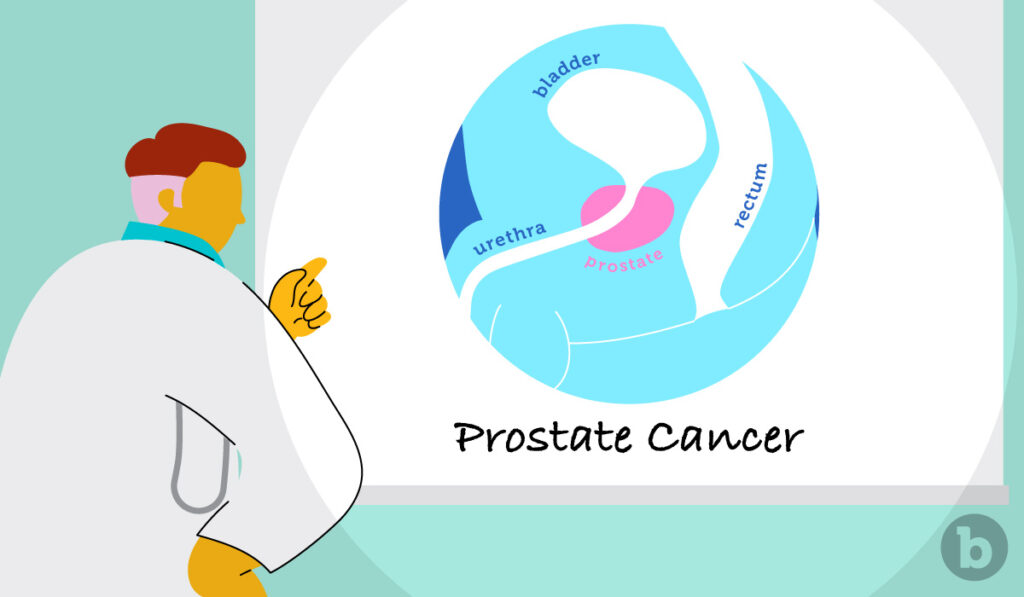
The prostate is a small, walnut-sized gland nestled between the base of the penis and the rectum, roughly two to four inches inside the anal canal. The rubbery gland plays a key role in reproduction, supplying prostatic fluid, which helps nourish and protect sperm from bacteria and other pathogens during ejaculation. The prostate contributes roughly 20 to 30 percent of the total semen volume, with the remainder supplied mostly by the seminal vesicles, which sit just about the prostate.
The prostate is a hard-working multi-hyphenate, playing a supporting role in hormone production and urine flow regulation as well. It is also a highly erogenous zone that can be accessed internally through the rectum, and externally via the perineum (AKA the taint or gooch), providing immense pleasure and an orgasm that research has described as "exceptionally pleasurable, often surpassing those obtained from penile stimulation."
An unfortunate statistic about the prostate is that it is one of the most commonly diagnosed cancers in men and people with penises. The American Cancer Society (ACS) estimates that 288,300 Americans will be diagnosed with prostate cancer in 2023 and that one in eight meant will be diagnosed with prostate cancer in their lifetime.
Given these concerning statistics, we wanted to spread awareness and share some vital information on prostate cancer, including how the cancer spreads, key risk factors, and how it can impair sexual function.
What is prostate cancer?
Prostate cancer is the second leading cause of non-skin cancer death in American men. Unfortunately, researchers still don't know precisely what causes prostate cancer, though they've identified some key risk factors.
Prostate cancer occurs when cells in the prostate develop changes in their DNA. These changes cause the cells to grow and divide more rapidly than normal. These abnormal cells tend to outlive others and eventually accumulate, forming a tumor. In time, some of these abnormal cells can break away, spreading to other parts of the body.
Many prostate cancers grow slowly and are confined to the prostate gland, where they may or may not cause serious harm. However, other types are aggressive and spread quickly to other parts of the body. As is true with most cancers, early detection is best for successful treatment.
In its early stages, prostate cancer may show no signs or symptoms. However, more advanced prostate cancer can show symptoms like: trouble urinating, blood in urine or semen, bone pain, weight loss, and erectile dysfunction. One should consider seeing a doctor if these signs are persistent, if they intensify, or if they begin to concern you. If prostate cancer runs in the family, doctors recommend getting your PSA (prostate-specific antigen) checked at age 50, and every few years after that.
What are some genetic, environmental, or lifestyle factors that can increase the chances of developing it?
Most prostate cancers are detected in older men and people with penises. About six in 10 cases are found in men who are 65 or older, with the average age of diagnosis being 66. It is considered rare to be diagnosed with prostate cancer under the age of 40.
For reasons that have not yet been determined, African American men and Caribbean men of African ancestry are at greater risk of prostate cancer than other races. These cases have also been found to occur in younger folks.
Diet is also suggested to play a role. For example, men who eat a lot of dairy products have a slightly higher chance of being diagnosed. Similar results have been found with those who consume lots of calcium. While some studies suggest obese folks are at higher risk of more aggressive forms of prostate cancer, they have a lower risk of being diagnosed with a slower-growing form of the disease. The specifics around these factors are still unclear, requiring further research to reach a more conclusive result.
Some studies suggest prostatitis (which is often caused when bacteria in the urinary tract enter the prostate) is linked to an increased risk of prostate cancer. The link between the two is not yet clear, but this is an active area of research, according to the ACS. Studies also suggest that men who've had a vasectomy have increased risk, though not all studies on the subject have reached this same conclusion.
As you can see, most of the data currently available are largely inconclusive and requires further research. However, the ACS says the best ways to reduce prostate cancer are to maintain a healthy weight, to keep physically active, and to follow a healthy eating regimen, with lots of fruit, vegetables, and whole grains while limiting red and processed meats, sugar-sweetened beverages and highly processed foods.
Generally speaking, anything that's good for your heart is good for your prostate.
How does prostate cancer affect sexual intercourse?
In rare cases, prostate cancer may cause erectile difficulties, but cancer itself does not usually affect sexual function. However, the treatment and surgery for this cancer can, especially in the first few months after treatment.
Because the prostate and seminal vesicles create semen, people who've had prostate surgery will begin having dry orgasms, meaning they can no longer ejaculate. Orgasms are still pleasurable, they're just different, as there won't be that familiar build-up sensation when reaching orgasm. Resources urge the importance of distinguishing orgasm from ejaculation during this time, as men will continue to have the sensations of orgasm without any physical evidence.
Because the nerves that control erections are so delicate, surgery or radiation for prostate cancer may damage them to the point that it causes erectile dysfunction (ED), meaning you cannot get or maintain an erection at all, or as easily as you used to. Resources share that up to half of men who have radiation for prostate cancer experience ED afterward, and in some men, these symptoms will improve over time.
Anal sex after prostate cancer is largely understudied. This is nothing new; we didn't even begin to study the prostate as a source of anal pleasure into 2014. In fact, multiple studies cite queer patients' discomfort when discussing their sexual orientation, since so few doctors inquire about it. And although anal sex is enjoyed by all genders and sexual orientations, it is still largely considered a niche act, or one reserved mostly for homosexual men.
With such little information available, b-Vibe reached out to urologist Dr. Justin Houman on how prostate cancer can impact butt stuff. "Generally speaking, men should abstain from receiving anal sex while being evaluated, diagnosed, and treated for prostate cancer," he says. "You can obviously have sex during that time, but at some points, it is advisable not to receive anal sex." Reasons for this vary, from potentially harming the area, to accelerating the spread of abnormal cells.
Houman adds that if you enjoy the feeling of a penis or toy rubbing against the prostate, people will no longer experience that sensation. "Once the prostate is not there, anal sex might feel different," he warns. But that's not to say anal sex won't be pleasurable. There are many nerve endings in our rectum and sphincter muscles, and that delightful feeling of fullness is still there. However, one study did not an "increase in pain and/or loss of pleasure in the rectum dramatically changed the experience of receptive anal sex in some men."
But this is only "some men," and the treatment outcome will vary by the individual. "Given our technology these days, rest assured, there are many ways to improve erectile function after prostate cancer treatment," Houman says. These include pelvic radiation, pharmacotherapies like Viagra and Cialis, and many other options that you can read more about here.
While the prostate does play a role in fertilization and sexual function, not having one does not mean you can no longer enjoy sex. It might just require a little more creativity which, as proud purveyors of anal products, we encourage.